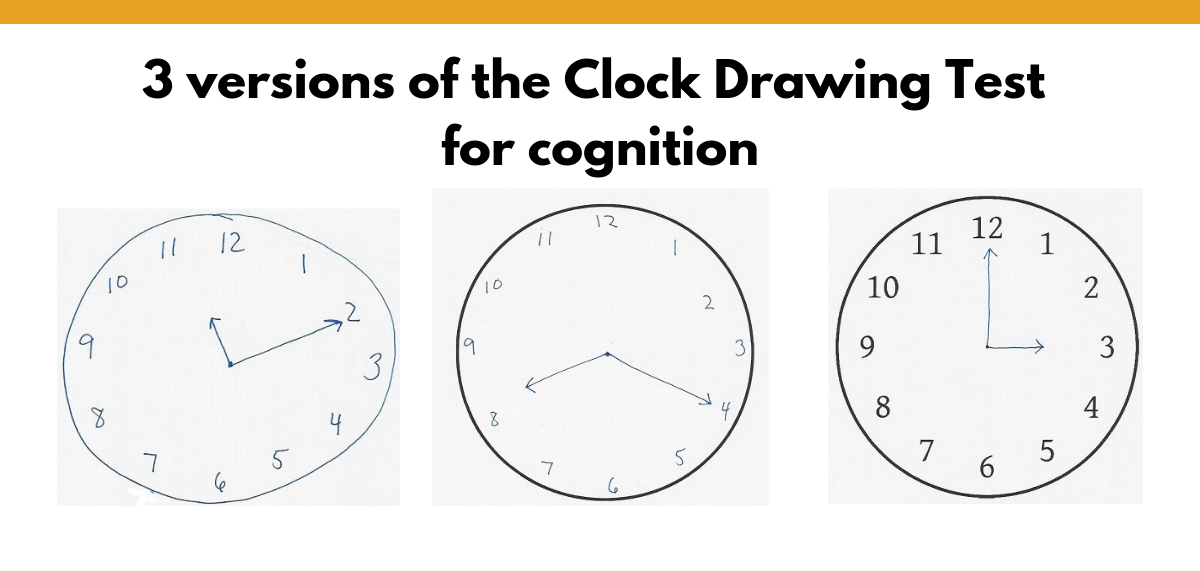
Michelle Dehgan, MA, CCC-SLP, BCS-S presented “The Utility of the Clock Drawing Test” at the 2018 ASHA Convention. She demonstrated three versions of the clock drawing test (CDT) and recommended we use all three to assess each patient to gain more insight into their cognitive status.
Michelle generously gave permission for me to share her handouts, and you can download her entire presentation. Her slide deck includes lots of great information, as well as interesting clocks drawn by patients.
Free DIRECT downloads: Clock Drawing Test – .doc, Clock Drawing Test – PDF, and scoring sheet. (cheat sheet). (Email subscribers get free access to all the resources in the Free Subscription Library.)
Outline:
- How you can use the Clock Drawing Test (CDT).
- The CDT assesses four main areas of cognition.
- Three versions of the CDT.
- Types of errors.
- Scoring systems.
- Using CDT results to guide therapy.
- My take-away.
- Related Eat, Speak, & Think posts.
- References.
How you can use the clock drawing test (CDT)
You can use the CDT as an assessment tool, an educational tool, a monitoring tool, and a planning tool.
- Assess specific cognitive abilities in people with neurological impairment.
- Detect early signs of dementia.
- Monitor decline in progressive neurological conditions.
- Detect improvement in people who’ve had a stroke or TBI.
- Use as an educational tool for patients and caregivers.
- Plan further assessment and treatment.
(Freedman et al, 1994)
The CDT assesses four main areas of cognition
You can gain insight into four main areas of cognition:
Spatial attention
Spatial attention is very complicated, and there’s not a universally-accepted theory about how it works. But we can understand that spatial attention is divided into two stages. First, we engage in simple spatial perception. In this first stage, we locate objects in space and notice features such as its dimensions, orientation, and distance. (Trojano & Conson 2008; 373)
In the second stage, we engage in complex spatial cognition. We use mental representations to understand the object and perform higher-level tasks such as recognizing shapes, learning mazes, or mental rotation. (Trojano & Conson 2008; 373)
If you want to assess visuospatial skills by themselves, you’d have to use simpler tasks than the CDT. Some example assessment tools for sale include the Benton Judgment of Line Orientation Test, the Visual Object and Space Perception battery, or the Battery for Visuospatial Abilities.
Just to give you an idea of what these tasks are, Trojano and Conson (2008) describe several visuospatial tasks, including:
- Judging line length and orientation.
- Comparing the width of angles.
- Judging whether a dot in a square is in the same position as the example.
- Pinpointing the location of a numeral in a square.
- Mentally rotating images.
- Recognizing nonsense shapes.
- Determining the number of cubes composing a complex three-dimensional shape.
- Mentally constructing images.
If your patient has impaired spatial attention, you may see visual neglect (usually left neglect), difficulty with positioning the numbers, and difficulty with the length and position of the clock hands. With the CDT, other impaired cognitive skills can cause these errors. (It’s hard to tease apart!)
Visuoconstruction
When we assess visuoconstruction skills, we’re looking to see how well a person can coordinate fine motor skills with spatial skills through drawing.
In order to draw a clock, a person must successfully use these visuoconstruction skills:
- Retrieve their mental representation of a clock.
- Create or retrieve a motor plan to draw the clock.
- Construct an accurate layout of the clock.
- Recall and place numbers in the correct location and orientation.
- Result should be a well-planned and organized clock face.
According to a clinical neuropsychologist, people who have trouble with visuoconstruction skills “often struggle with daily tasks such as arithmetic, driving, and writing.”
Impaired ability to draw a complex shape, such as a clock, is often called “constructional apraxia” or CA. (Trojano 2012)
Symbolic representation
Through the CDT, your patient demonstrates their understanding of how to represent time with a drawing. You can assess their symbolic representation of the 12 numbers, as well as the hour and minute hands set to represent the time.
Executive function
Drawing a clock requires use of multiple executive function skills, including:
- Comprehending and remembering verbal or written instructions.
- Developing an organized, multi-step plan of action.
- Using self-monitoring skills to follow the instructions.
- Simultaneously recalling and writing numbers while maintaining the spatial layout of the clock.
- Detecting and correcting errors.
- Inhibiting any impulse to continue beyond the directions.
- Attending to a difficult task
- Tolerating frustration if it’s a difficult task.
(Freedman et al, 1994)
Three versions of the CDT
Michelle’s recommendation is to administer all three versions of the CDT, which takes about six to 10 minutes. We should administer them in the order presented here, from least-structured to most-structured.
Download Michelle’s assessment materials
Download Michelle’s assessment materials (or PDF version). I lightly edited it by providing the circle for the pre-drawn condition and renaming the tests to be consistent with her presentation and for clarity. This five-page download includes all the pages you’ll need for the following three CTD versions.
Free-drawn Clock
The Free-drawn Clock is the most challenging version. You hand a blank piece of paper to your patient and ask them to draw a clock. You may choose to give the directions all at once or break into two steps, depending on how much you want to tax your patient’s memory. These instructions come from Michelle’s presentation (you can substitute the time of your choice).
Instruction A – directions given all at once:
- “Draw the face of the clock, put in all the numbers, and set the time to 10 after 11.”
Instruction B – break the task into two steps:
- “I’d like you to draw a large circle and fill it in with numbers like on the face of a clock. Make it large enough so that a child could read it.”
- “Now place the hands on the clock so that it reads 10 after 11.”
Pre-drawn Clock
The Pre-drawn Clock version is easier because the circle representing the clock face is already drawn. You would ask your patient to add all the numbers of the clock and set it to your desired time.
Examiner Clock
The Examiner Clock is the easiest version. In this version, you’d give your patient three clocks already drawn and ask them to add the hands to represent three separate times. You may use any times you like, but the following are commonly used:
- “10 after 11” is most sensitive to neurocognitive dysfunction (Kaplan).
- “20 after 8” is common in neurology.
- “3 o’clock” as a simple time.
Types of errors
Michelle lists six types of errors to consider:
- Size of the clock.
- Graphical difficulties.
- Stimulus-bound response.
- Conceptual deficits.
- Spatial/planning deficits.
- Perseveration
The size of the clock should be between 1.5 inches and 5 inches in diameter.
Graphical errors include wavy lines, distorted clock face, numbers that are difficult to read, or hands that don’t meet.
A stimulus-bound response is “the tendency of the drawing to be dominated or guided by a single stimulus, most often related to the time-setting instructions.” An example is pointing the hands to the 10 and the 11 when asked to set the time for 10 after 11. If your patient does this, they are having difficulty suppressing the wording of the stimulus (your instruction) to arrive at the conceptual knowledge of 10 minutes past the hour of 11.
Conceptual deficits are “defined as a loss or impairment in accessing knowledge of the attributes, features, and meaning of a clock.” Michelle points out that the drawing may not look like a clock, or the hands don’t represent a time.
Spatial and planning deficits would show up as impaired placement of the elements of the clock.
Perseveration could show up as repeated numbers, numbers that extend past 12, or too many clock hands.
Michelle also goes into the common types of errors according to diagnosis, including Huntington’s disease, delirium, vascular dementia, Alzheimer’s disease, Parkinson’s disease with and without dementia, traumatic brain injury (TBI), Schizophrenia, metabolic syndrome, hepatic encephalopathy, and stroke broken down by area of damage. It’s beyond the scope of this post to go into that, but you can access her slides on ASHA’s 2018 Convention page.
Scoring systems
There are at least 13 published scoring systems, ranging from very simple to in-depth analysis. Michelle provided this handout which describes five scoring methods with examples. In her slide deck, she goes into detail on two scoring methods: Shulman’s 6 point scale and the CAMDEX scoring system.
Bear in mind that age and level of education do impact a person’s ability to draw a clock. Michelle reported on a study by Freedman et al which demonstrated that people over the age of 80 with normal cognition do make errors in drawing a clock. In addition, error patterns are different for people who have less than five years of education.
Using CDT results to guide therapy
When planning intervention, we want to look at the entire picture. We should consider:
- The needs, concerns, and goals of our patient and their loved ones.
- The diagnosis and prognosis for recovery.
- Our patient’s strengths and weaknesses.
- What further assessment should we do?
If our patient has an impaired ability to complete the CDT, we can gain insight into the nature of the problem. Is it attention, visuospatial, symbolic representation, and/or executive function? For instance, we may decide to work on attention, impulse-control, self-monitoring, abstract thinking, or judgment.
Michelle suggests that we use therapy tasks that incorporate visual, verbal, and tactile stimuli. She suggested that if our patient is easily distracted, that eliminating one sensory system may help them stay on task. She also provides sample goals in her slides.
My take-away
I thought this was a very interesting presentation with a lot of useful information. It’s interesting that research has shown that people with normal cognition do make mistakes on drawing a clock, especially older people. I also didn’t know that people with normal cognition but less than 5 years of education make different types of errors.
Learning about different scoring methods, as well as typical error patterns according to diagnosis was also fascinating.
My plan is to start assessment with the free-drawn CDT and if there are any errors to move on to the other two versions to provide additional information.
My impression is that if my patient can free-draw a clock and set the time to 10 after 11, then I probably wouldn’t get additional information from administering the two easier versions.
What do you think about using three versions of the CDT? Please leave a comment and share with your co-workers
Related Eat, Speak, & Think posts
- 18 free assessment tools for cognition.
- Single-use cognitive evaluation folders.
- How to assess pragmatic skills in adults with brain injury.
References
Freedman M, Leach L, Kaplan E, Winocur G, Shulman KI, Delis D. Clock Drawing: A Neuropsychological Analysis. New York: Oxford University Press; 1994.
Trojano, L., & Conson, M. (2008). Chapter 19 Visuospatial and visuoconstructive deficits. Handbook of Clinical Neurology, 88, 373-391. https://doi.org/10.1016/S0072-9752(07)88019-5
Trojano, L., Fragassi, N. A., Chiacchio, L., Izzo, O., De Cesare, G., Cristinzio, C., & Grossi, G. (2004). Relationships between constructional and visuospatial abilities in normal subjects and in focal brain-damaged patients. Journal of Clinical and Experimental Neuropsychology, 26(8), 1103–1112. https://doi.org/10.1080/13803390490515522
Free DIRECT downloads: Clock Drawing Test – .doc, Clock Drawing Test – PDF, and scoring sheet. (cheat sheet). (Email subscribers get free access to all the resources in the Free Subscription Library.)
Lisa earned her M.A. in Speech-Language Pathology from the University of Maryland, College Park and her M.A. in Linguistics from the University of California, San Diego.
She participated in research studies with the National Institute on Deafness and other Communication Disorders (NIDCD) and the University of Maryland in the areas of aphasia, Parkinson’s Disease, epilepsy, and fluency disorders.
Lisa has been working as a medical speech-language pathologist since 2008. She has a strong passion for evidence-based assessment and therapy, having earned five ASHA Awards for Professional Participation in Continuing Education.
She launched EatSpeakThink.com in June 2018 to help other clinicians be more successful working in home health, as well as to provide strategies and resources to people living with problems eating, speaking, or thinking.


Hello! Thanks for the excellent and attractively presented content! It looks like Michelle’s ASHA presentation is password protected now?
Yes, you’re correct. I had to log in with my ASHA password just now to access the seminar materials. I don’t recall if a log-in was required when I wrote the post, that was a few years ago! I don’t have permission to share her entire presentation.
If you’re not an ASHA member, perhaps you could try emailing her. I haven’t been in contact with her since I wrote this post. At that time, she was TIRR Memorial Hermann. (And thanks for the kind feedback!)