Curious about the real challenges and rewards of home health speech therapy (HH ST)? I surveyed both HH SLPs and those who’ve never set foot in a patient’s home to uncover the truths behind the myths. From the number of visits to the satisfaction with outcomes, my findings reveal surprising insights that challenge common perceptions and shed light on the unique aspects of HH ST. Respondents were informed that their answers may be shared anonymously on this site or in the continuing education course I presented in April 2024. Some of these findings surprised me, and they may surprise you, too!
Free DIRECT download: Home health SLPs talk about their job (info sheet). (Email subscribers get free access to all the resources in the Free Subscription Library.)
Outline:
- About the home health speech therapy (HH ST) surveys.
- Overview of respondent characteristics.
- Typical number of HH ST sessions.
- Satisfaction with # of HH ST visits.
- Do patients improve with HH ST?
- Do HH SLPs accomplish much?
- Transitioning to out-patient ST.
- Perception of why HH SLPs like their job.
- Why some SLPs won’t work in HH.
- What HH SLPs say about misconceptions.
- HH ST is not all roses and sunshine.
- Why many HH SLPs like their job.
- My thoughts and thank you!
- Want to learn more about the surveys?
- Related Eat, Speak, & Think posts.
About the home health speech therapy surveys
I was invited to put together a two-hour continuing education course for MSCC, which I presented on April 10, 2024. The coordinator asked me to include a section to dispel myths about HH ST. As I was thinking about how to do that, I quickly realized that using my own experience to discount “myths” would be highly subjective.
So I put together a survey for HH SLPs to share their experiences. After a couple of months of collecting survey responses, the MSCC coordinator suggested running a similar survey for SLPs who had never worked in home health. I thought that was a great idea. In fact, I wish I had thought of it at the start! I would have written some of the questions differently.
Regardless, she ran that survey until a technical issue deleted most of the data less than two weeks from when my course slides were due. I scrambled to recreate the “Perceptions” survey and asked for volunteers to fill it out. I managed to get 48 responses in 10 days! (Thank you to everyone who responded to either survey!)
These surveys are purely informal, designed to generate points of discussion regarding the “myths” of home health speech therapy.
Overview of respondent characteristics
The “Perceptions” survey:
- 48 speech-language pathologists completed the survey.
- None had ever provided therapy in the home.
- Variety of work settings.
- 47 work in the US, 1 works in Canada.
- Responses collected 3/16/2024 – 3/26/2024.
The “Experience” survey:
- 155 home health SLPs (1 works mobile outpatient).
- 153 are based in the US, 1 from Canada, 1 from UK.
- Responses collected between 11/29/2023 – 3/26/2024.
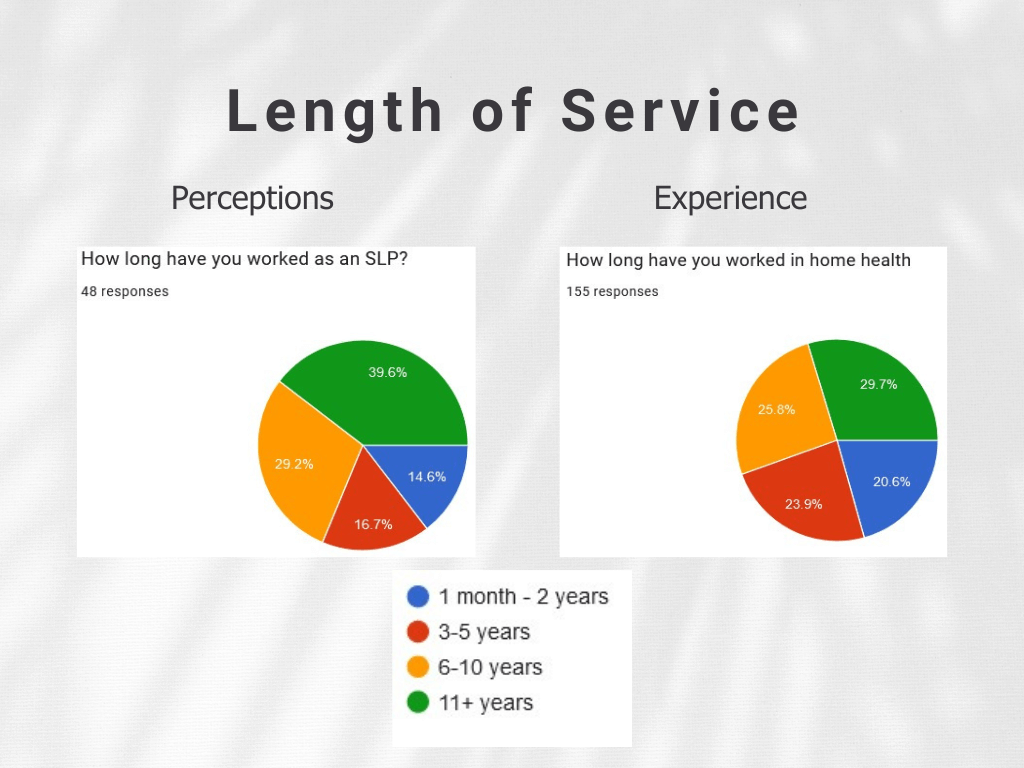
Years of service as an SLP
I asked the non-HH clinicians how long they’ve been an SLP. I asked the HH clinicians how long they’ve worked in home health.
You can see there’s a nice distribution of years of service in both groups, keeping in mind that it’s likely the HH SLPs also worked in other settings.
In retrospect, I should have asked the HH clinicians how long they’ve been an SLP. I should also have broken the 11+ years into at least one more level. However, you can see that there is a nice spread of years of service in both groups.
Typical number of HH ST sessions
Next I asked about the typical number of speech therapy sessions in home health. I know this is a hard question to answer, but I wanted to explore the idea that patients don’t receive many HH ST visits as a rule.
Survey questions:
- Perceptions survey: “How many ST sessions do you think the typical home health patient receives?”
- Experience survey: “How many therapy sessions do you typically conduct with your home health patients?”
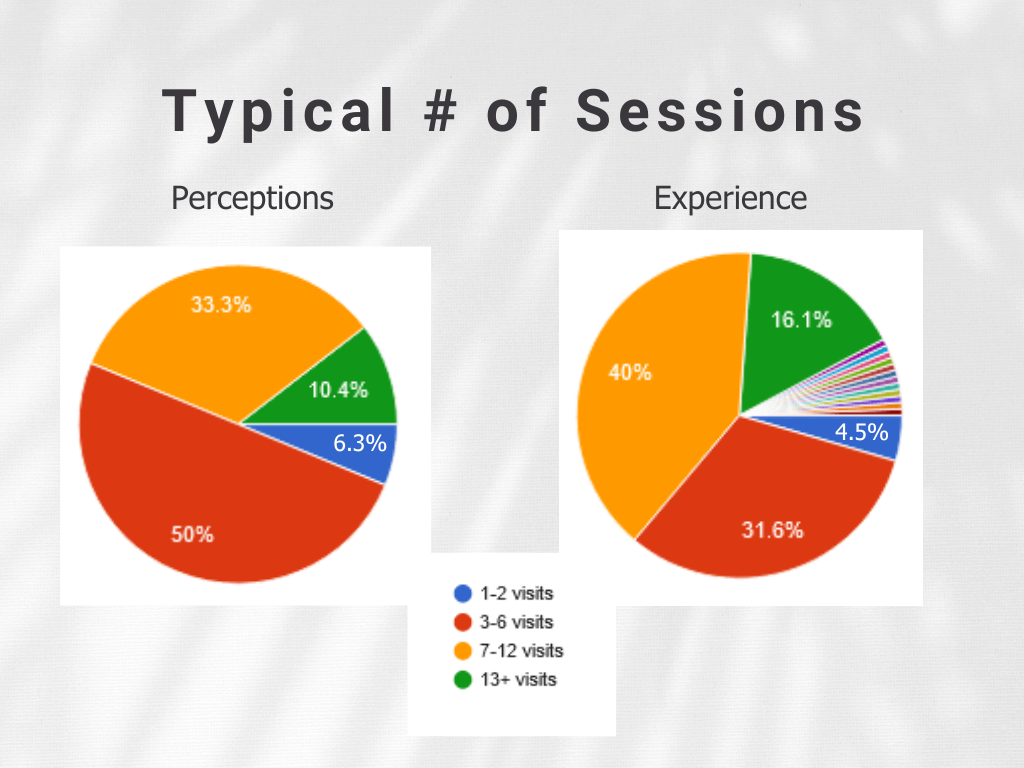
In comparing the two charts, we can see that non-HH clinicians tend to believe that patients receive fewer HH ST visits than the Experience survey indicates. Starting at the low end of the scale (looking at blue and red), 56.3% of non-HH clinicians believe patients typically receive 6 or fewer visits. Compare that to 36.1% of HH clinicians reporting that they typically offer 6 or fewer visits to their patients.
Wondering what all those colorful slices are in the Experience survey? I allowed respondents to choose “other” and write in their own answer. Those are pretty much all variations of “it depends”.
If HH ST visits are limited, what is the reason?
I asked a follow-up question on the Experience survey: “If you have to limit the number of visits, what are your reasons?” The top 5 answers were given as “select all that apply”, but I also allowed people to write in an “other”, which is the rest of the chart. We’ll just focus on the top portion of the chart here.
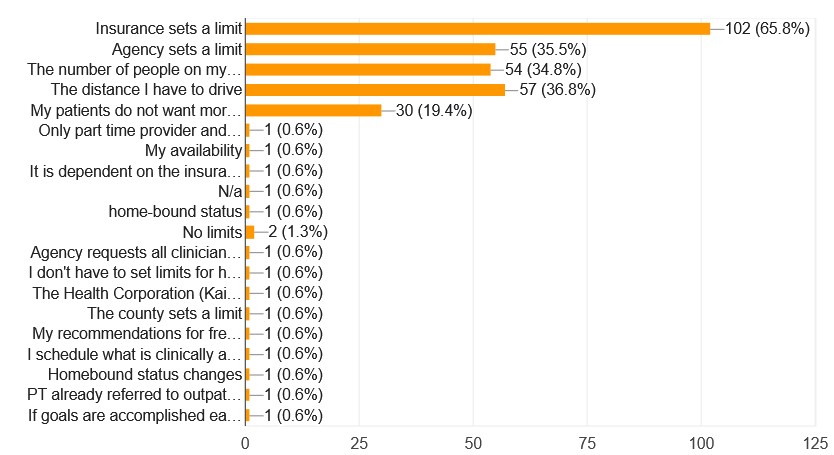
I don’t think any of us are surprised that some insurance companies set a limit on the number of visits, but I was surprised that 35.5% of HH SLPs reported that their agency sets a limit. Social media comments suggest that some clinicians think that PDGM mandates that rehab visits are limited and divided among the disciplines. It’s worth keeping in mind that 64.5% of HH SLPs did not check off the “agency sets a limit” box.
Satisfaction with # of HH ST visits
I know from my own experience that SLPs can accomplish highly meaningful outcomes with just a few sessions. I’ve written about two such cases, such as this cognitive case study and this reluctant patient. In other words, fewer sessions does not necessarily mean worse outcomes. So I asked about satisfaction with number of HH ST visits.
Survey questions:
- Perceptions survey: Do you think home health SLPs are satisfied with the number of visits they can provide?
- Experience survey: Are you satisfied with the number of visits you can provide?
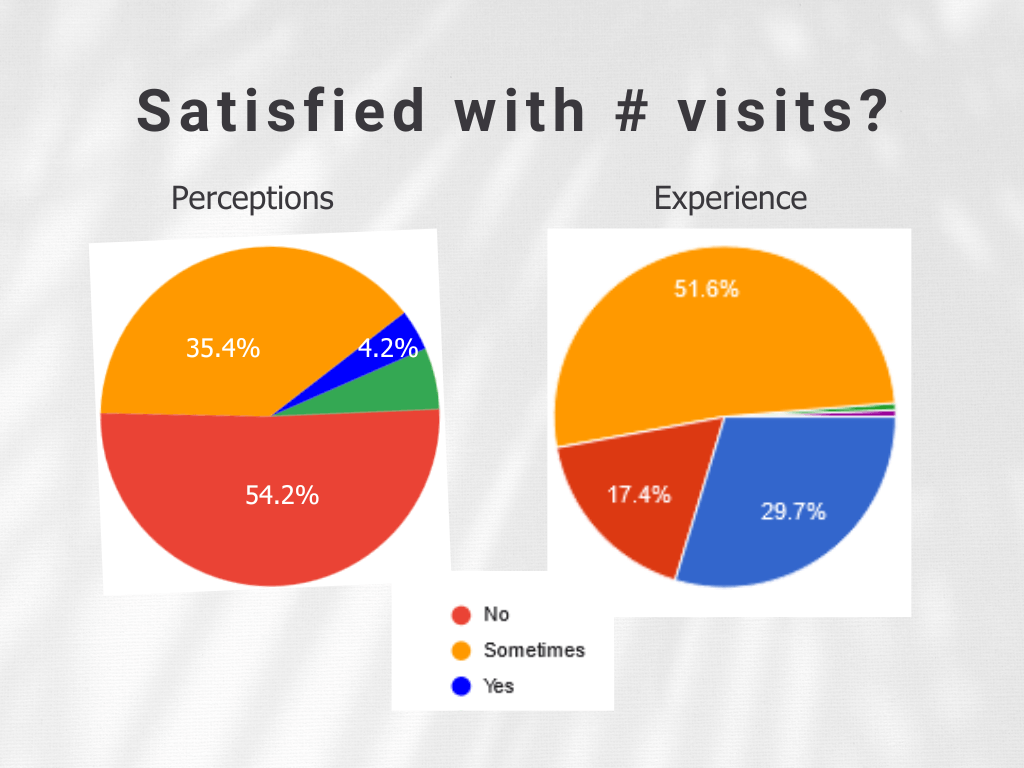
A “yes” answer is blue. Only 4.2% of non-HH SLPs thought that HH SLPs are satisfied with the number of visits they can offer. Compare that to the 29.7% of HH SLPs who report satisfaction with number of visits.
Notice also that 54.2% of non-HH SLPs thought that HH clinicians are NOT satisfied with the number of visits they can provide, compared to 17.4% of HH clinicians reporting dissatisfaction.
Do patients improve with HH ST?
Next comes an important question. Do patients show improvement with HH ST?
Survey questions:
- Perceptions survey: Do you think home health patients typically show meaningful improvements in their ST goals by the time they are discharged?
- Experience survey: Do your patients typically show meaningful improvement in their ST goals by the time you discharge?
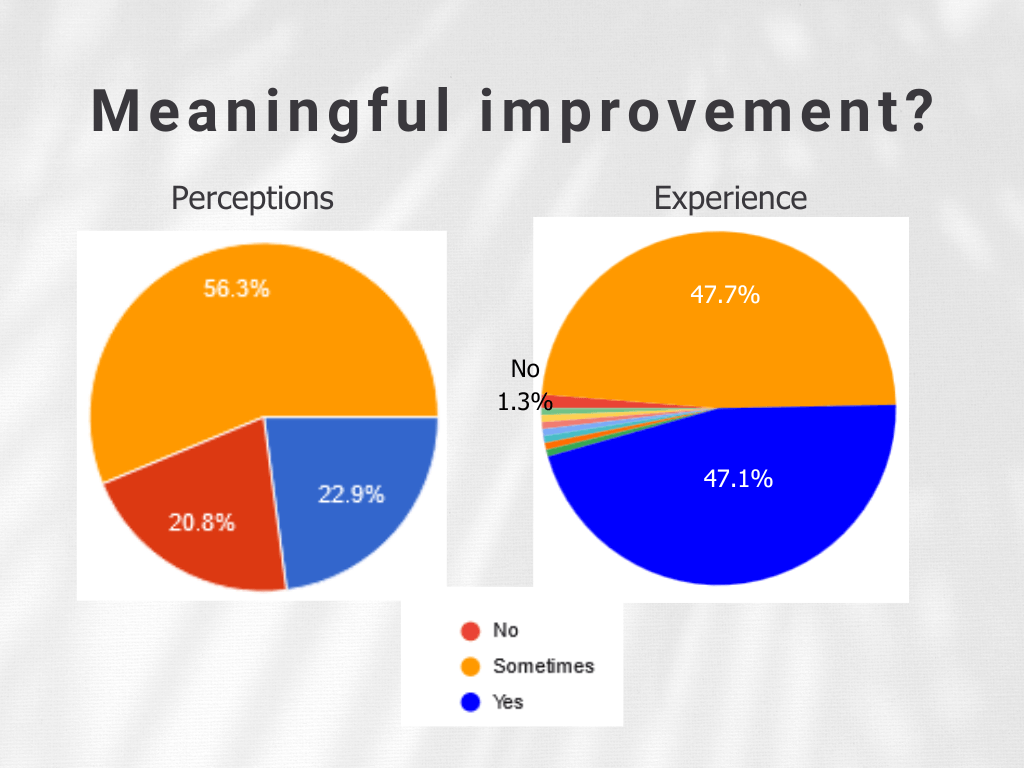
Ideally, we would want to see a “yes” answer, which is blue in the charts. On the Perceptions survey, only 22.9% of clinicians think patients improve with HH ST. In contrast, 47.1% of HH SLPs report that they patients typically show meaningful improvement by the time they discharge.
On the flip side, 20.8% of non-HH clinicians think patients don’t benefit from HH ST (10 out of 48 responders). Compare this to 1.3% of HH clinicians who also responded “no” (2 out of 155 responders).
The Experience survey includes other colorful slices due to respondents choosing “other” and writing in their own answers, generally to explain “sometimes”.
Do HH SLPs accomplish much?
I’ve heard comments online that suggest that HH SLPs don’t really accomplish much, so I wanted to dig into this idea further.
Survey questions:
- Perceptions survey: Do you believe the perception that home health SLPs “don’t accomplish much” is accurate?
- Experience survey: Do you believe the perception that home health SLPs “don’t accomplish much” is accurate in your experience?
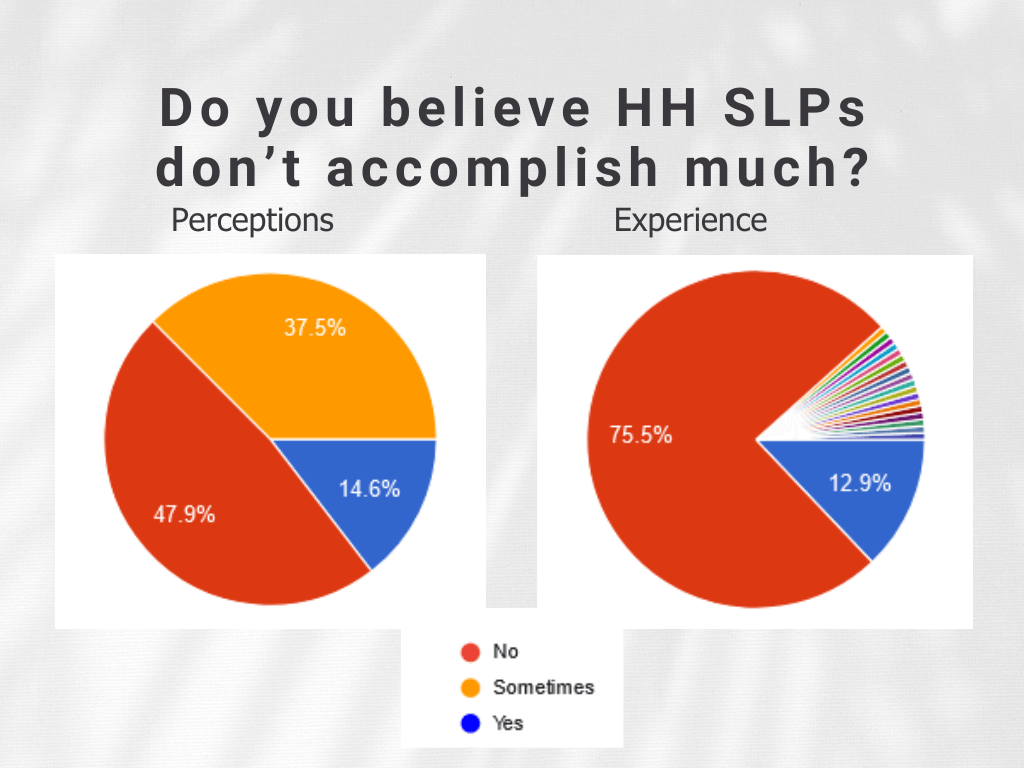
Ideally, we would hope to see “no” (red). At a quick glance, we can see a lot more red on the side of HH SLPs. I was actually surprised to see that nearly 50% of non-HH clinicians reported that they did not believe this statement. It’s also interesting to see that a nearly equal percentage of both groups reported that they did believe it.
Again, all of the colorful slices on the Experience chart are variations of “sometimes”. Here are a few quotes:
- I feel it is now more than ever [true] due to the limitations.
- Sometimes! I feel limited by the resources I have sometimes.
- Sometimes that’s true, but it’s highly dependent on whether there are available and willing caregivers to follow through with your instructions.
- Sometimes. Those of us who really lean in to adult education, I think we are effective, but getting a transplant from a school or a hospital, where handouts and flashcards are the norm makes it difficult for the transition for a good percentage of us I think.
Transitioning to out-patient ST
One of my own misconceptions was that patients generally transitioned to out-patient to continue ST. In my experience, far less than half of my patients go on to OP. But I’m just one person, so I put this question to my colleagues.
Survey questions:
- Perceptions survey: Do you think home health patients generally transition to out-patient therapy?
- Experience survey: Do your patients generally transition to out-patient therapy?
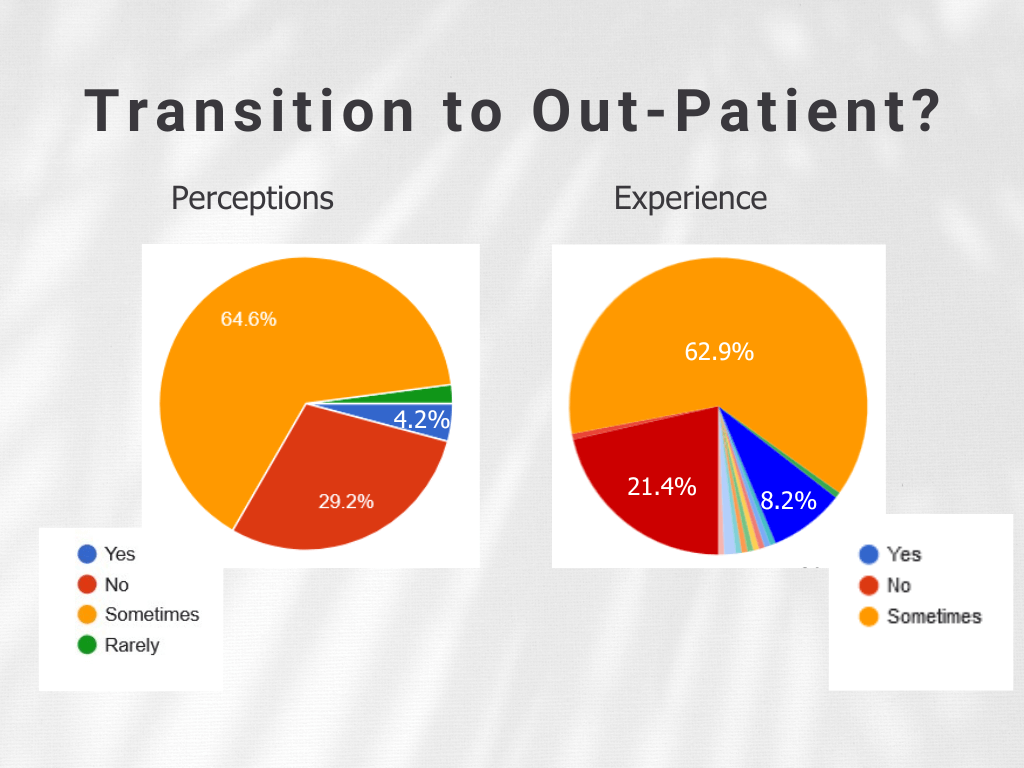
These responses are relatively similar, although a larger percentage of HH SLPs said “yes” (blue) compared to non-HH SLPs.
Perception of why HH SLPs like their job
Another possible misconception I’ve heard is that some SLPs like working in HH because it is easier than other settings. So I asked the non-HH SLPs the following question: “Why do you think some SLPs enjoy working in home health?”
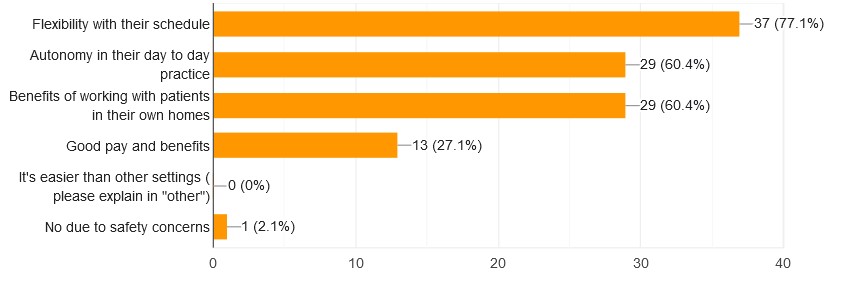
In the chart above, we can see that more than half of non-HH SLPs believe that main factors are flexibility with their schedule, autonomy in day-to-day practice, and the benefits of working with patients in their own homes.
No one reported believing that HH is an easier setting than others, which is nice to see! I have seen this sentiment on social, though, but maybe it’s more of a minority view. HH is by far the most challenging setting I’ve worked in, but that’s just my opinion. Unfortunately, I didn’t ask the HH SLPs what they liked about their jobs.
Why some SLPs won’t work in HH
Finally, I wanted to bring up some other misconceptions I’ve heard. I asked the non-HH SLPs the following question: “Why do you think some SLPs would never work in home health?”
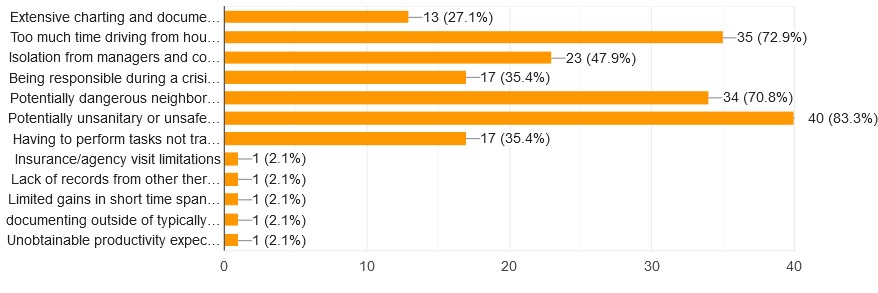
The non-HH SLPs cited the following top 3 reasons why some SLPs avoid working in HH:
- Potentially unsanitary or unsafe homes: 83.3%
- Too much time driving from house to house/large territory: 72.9%
- Potentially dangerous neighborhoods: 70.8%
What HH SLPs say about misconceptions
I asked the HH SLPs a similar question, “What do you think are the most significant misconceptions about working in HH?” As I set this up as an open-ended question, I received 155 different responses. So, no handy chart to show.
Here are some quotes from the Experience survey.
Cleanliness and safety
What HH SLPs say are misconceptions about cleanliness and safety:
- It’s dirty and unsafe.
- That homes are dirty.
- It is gross.
- That it’s significantly dangerous. There are some dangers, but the majority of the time I feel safe.
- That we are in unsafe situations or dirty environments most of the time.
- That we are in unsafe/dirty environments all day. I think those homes are the outliers.
- Fear to go into homes: most people are so warm and grateful to have help.
Drive time/territory size/workload
What HH SLPs say are misconceptions about drive time/territory size/workload:
- The drive time is terrible. Not if you work for a great company!
- That it’s easy and lucrative.
- That it’s the easiest placement.
- Lots of traveling, short visits, limitations to visit numbers.
- That even new grads can be effective in home health therapy.
- Too much paperwork.
- That it’s similar to outpatient treatment.
- That HH SLPs are not especially skilled.
Achieving meaningful outcomes
What HH SLPs say are misconceptions about achieving meaningful outcomes:
- That patients don’t improve.
- That you can’t accomplish anything.
- That we don’t do anything.
- We don’t do “real” therapy.
- That we don’t help our patients.
- That often times we educate and then discharge. The expectation is to transition to outpatient, which is not the reality.
- I used to think home health therapists (ot,pt,st) were “the bottom of the barrell” but I know better now. They’re the experienced, knowledgeable backbone of rehab.
HH ST is not all roses and sunshine
Many of the issues above are listed as misconceptions by some HH SLPs, but other HH SLPs did say that some of those issues are real for them. Here are some quotes from the Experience survey:
- It has gotten harder since PDGM started.
- I’m frustrated by the lack of interaction with other SLPs.
- The amount of documentation needed for a single visit is absurd.
- I found the number of visits and distance required to travel negatively impacted the amount of time and energy I had to increase my knowledge and skills to benefit my patients.
- Sometimes I feel like I am driving more than seeing patients and the days can be long. Work and home balance is non-existent.
- No one really prepared me for the duties of case managing in HH. So much is required that sucks time from working at the top of my license.
- The oasis is not geared toward ST at all. Nurses get to decide if ST (or PT/OT) is needed. They are not therapists. It is all about money. We were literally told (when discussing visits are a pt) that ”well this is a business.”
- It has gotten harder to treat patients. Medicare PDGM I feel screws SLPs. PT gets in first and takes the majority of visits. No one usually cares about speech. It’s a shame. Also, patients are sicker post Covid pandemic. Constant re hospitalizations affecting progress.
- The driving and distances are the worst part. I cannot make nearly the same amount of money my PT counterparts make, because my patients are usually 20 to 60 minutes away which means there is a limit to how many visits I can make within a workday. I refuse to work 10 hour days at this stage of my career, so I settle for much less money.
- It is very hard to get MBSS/FEES or even additional records. When patients have good support they tend to do well. When they don’t, or if they are very very low SES, they tend to struggle much more.
- There are so many requirements per visit that it takes away from therapy time. (Taking vitals, asking required questions every time, paperwork… unrelated duties to speech therapy).
- The biggest struggle is lack of equipment access. Like I cannot get Breathers, EMST, vital stim, IOPI, or any of those kinds of treatments. There is not nearly as much collaboration between disciplines as I would like.
Why many HH SLPs like their job
I did not ask HH SLPs what they liked about their job, but many respondents on the Experience survey shared their thoughts. Here are some quotes:
- Love the flexibility.
- It is very flexible and nice that no one bothers me about productivity
- Working in HH is “more controlled and safer” than expected.
- The effectiveness of treatment can actually be increased because therapy is being conducted in a familiar setting with access to meaningful and relevant materials (e.g., patient’s own meds and pill box, own calendar, etc.)!
- You can accomplish a TON of meaningful, functional goals as a speech therapist in home health. I feel much more helpful and impactful doing real things in the person’s actual environment than I ever did working at the SNF.
- I love it. I tell every company at interview that I WILL NOT compromise how often I see someone for profits, but that when insurance cuts them off, obviously I know I can’t go over. I’m reasonable and very very rarely get any push back.
- I love being able to work on functional goals and caregiver education. You often can’t do that in other settings.
- I’m 30+ years in, and this is my favorite setting… I set my own frequencies based on clinical judgment. My visits can be as long as I need them to be and are longer than most therapists in my agency.
- Home Health is the most engaging and rewarding experience I have had in my career, to be able to see the patient in their own environment has been challenging, fulfilling, rewarding, but it is also where patients I feel excel.
- The home health company is what makes you or breaks you. My prior company was profit over people and constantly fought me to reduce the number of visits. My current company is ethical, reasonable, and while they still need to stay in business, they absolutely respect my clinical judgment and autonomy.
- I love home health. I work for a good company with wonderful local managers who are supportive. This survey is making me appreciate how lucky I am! I currently have two patients on caseload with aphasia and apraxia with whom I’m probably nearing 100 visits each. One is an hour drive away from the office and most of the rest of my caseload. But they both continue to make gains, are definitely home bound, and are nowhere near baseline. Not one complaint or question from management!
My thoughts and thank you!
The surveys highlight that providing speech therapy in the home is both challenging and rewarding. Despite the very real challenges that HH SLPs face, there are misconceptions about the setting and the clinicians who work in HH. Unfortunately, the misconceptions aren’t based on myth, but perhaps the problems are not as dire or as prevalent as commonly believed.
I hope that this survey helps non-HH realize that there may be more to HH than they believe. And I hope the survey makes it clear to all SLPs that the experience of working in HH can be vastly different depending on the company you work for and your geographic location.
My surveys only focused on a subset of potential problems in HH, specifically, the problems that I felt were more misconception and less reality. I found the responses to be enlightening and at times surprising. I truly appreciate everyone who responded!
If people are interested, I could create a new survey to more fully explore the HH ST experience. Just comment below or respond to any of my newsletters!
Want to learn more about the surveys?
I share more information about the surveys in “What Really Happens When Patients Go Home”, a 2-hour CE course available to members of MSCC (recorded). For instance, I compare what non-HH and HH SLPs say about the reasons for the number of ST visits that are provided. I also compare what each group feels about why HH patients don’t show more improvement. And I share more on the challenges and benefits to HH ST. The surveys are a small part of the CE course, which focuses on how to achieve meaningful outcomes in any setting. (I don’t want to misrepresent the CE course as a deep dive into these surveys!).
Related Eat, Speak, & Think posts
- 50 questions to ask in a home health SLP interview.
- 17 tips for the new home health SLP.
- Home health SLP survey results may surprise you.
- My best day as a home health SLP.
- My worst day as a home health SLP.
Free DIRECT download: Home health SLPs talk about their job (info sheet). (Email subscribers get free access to all the resources in the Free Subscription Library.)
Featured image by iKrUeMeL from pixabay, found on Canva.com.
Lisa earned her M.A. in Speech-Language Pathology from the University of Maryland, College Park and her M.A. in Linguistics from the University of California, San Diego.
She participated in research studies with the National Institute on Deafness and other Communication Disorders (NIDCD) and the University of Maryland in the areas of aphasia, Parkinson’s Disease, epilepsy, and fluency disorders.
Lisa has been working as a medical speech-language pathologist since 2008. She has a strong passion for evidence-based assessment and therapy, having earned five ASHA Awards for Professional Participation in Continuing Education.
She launched EatSpeakThink.com in June 2018 to help other clinicians be more successful working in home health, as well as to provide strategies and resources to people living with problems eating, speaking, or thinking.


Be First to Comment