These three home health SLP survey results may surprise you! I’ve seen in online forums that some clinicians love home health, while others face a lot of challenges, so I wanted to get a closer look at the situation with a survey.
The participants were informed that their answers may appear on my blog or in a continuing education course. I also ran another survey asking SLPs who’ve never worked in home health to share their perceptions of home health speech therapy, but those results aren’t discussed below.
Outline:
- About the home health SLP survey.
- Satisfaction with number of visits.
- Limitations on number of visits.
- Enough to meet patients’ needs?
- Improving participation-focused intervention.
- Learn more about the surveys.
- Related Eat, Speak, & Think posts.
About the home health SLP survey
The “Home Health SLP Experience Survey” is an informal survey that was open for responses between 11/29/2023 and 3/26/2024.
It was completed by 155 home health SLPs (one reported working in mobile outpatient therapy), 153 based across 42 states in the US, 1 in Canada, and 1 in the UK.
A big thank you to everyone who participated!!
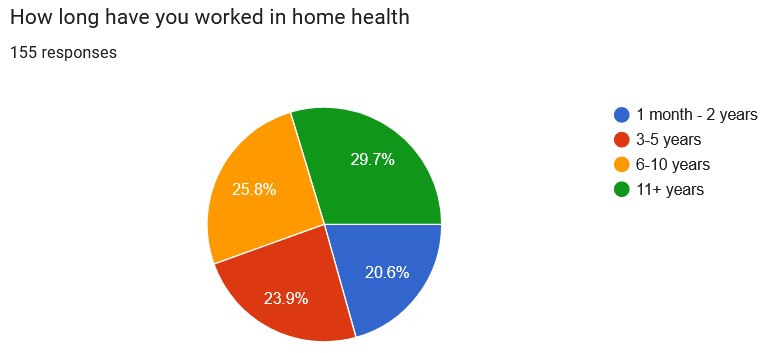
There’s a nice distribution of length of service:
Satisfaction with number of visits
One question I wanted to ask was whether home health SLPs were satisfied with the number of visits they could provide.
Looking at the pie chart below, we can see that roughly 30% of clinicians said they’re satisfied, while 17% reported they are not satisfied. Half of clinicians said they were “sometimes” satisfied.
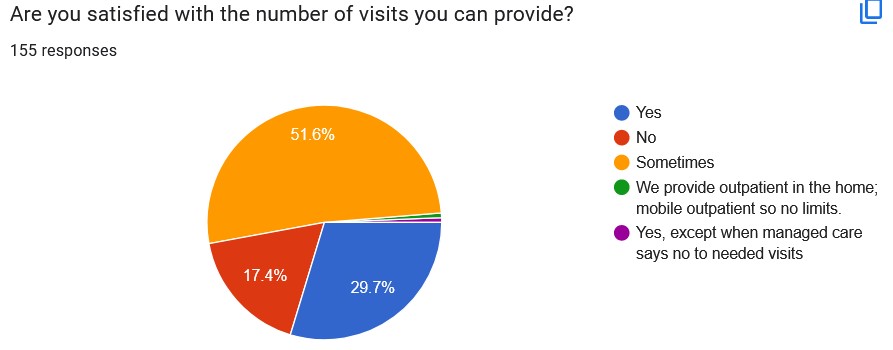
Being an SLP is hard work, no matter what setting we’re in. I think the primary reason we persist in demanding jobs is because we want to help patients. When our visits are constrained by factors out of our control, it just puts added stress on us and presumably decreases our effectiveness. I’d love to see that 30% satisfaction rate increase.
One of my goals this year is to implement participation-focused therapy and share what I’m learning. While we may be able to advocate for more visits for our patients, there are many factors that are out of our control. Perhaps by changing our focus in the sessions, we may increase our satisfaction and improve our patients’ outcomes.
Let’s talk next about what is limiting the number of visits.
Limitations on the number of ST visits
I’m sure that you can already guess many of the factors which limit the number of ST visits. One finding in particular surprised me, and it may surprise you as well.
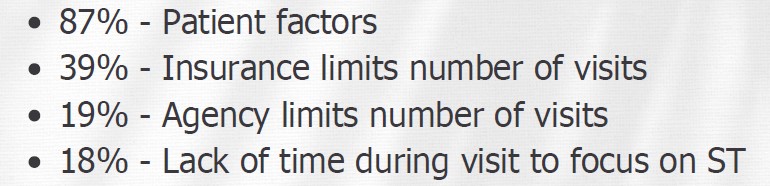
Here are the four most common reasons for the limit on the number of home health ST visits. Respondents could select as many answers as they wanted.
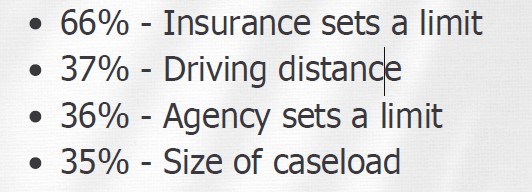
Other reasons included the patient not wanting more visits, patients going on to outpatient, and agency declining to increase the SLP’s working hours.
I think many clinicians may find it surprising that some home health agencies set a limit on the number of visits. My agency does not set a limit, so I was dismayed when I started hearing chatter online from other SLPs.
But even the SLPs who work under agency limits may be surprised to learn that they are in the minority, at least according to this small survey. Agency limits on ST visits is not a mandated part of PDGM.
Comments from SLPs with agency limits
Many SLPs shared that the total number of therapy visits are capped, and some said that they can’t evaluate until PT/OT discharge.
Here are some comments regarding the number of visits:
- 19 total for 3 disciplines over 60 days.
- 20 visits between all disciplines.
- My agency typically allows for no more than 12 visits (2wk6).
- If all 3 disciplines are in, I generally only get a few visits.
- Limited visits when other disciplines are involved.
- We are limited to 1 a week, unless I really feel like they need 2.
- They say go less than a month.
- If all 3 therapies, then ST usually gets 1 wk 4 while OT/PT get 2 wk 4 for total of 20 visits.
- Shared total number of visits with other disciplines if we are all seeing the patient. 16 visits total in first 30 days, 12 visits total second 30 days.
- They primarily will put in PT before ST and only want 1 discipline in at a time. Since they want to recert for a second time, then they will add another discipline if it benefits them.
And here are comments regarding PDGM specifically:
- PDGM.
- Company uses a software program to dictate how to spread out 12 visits across all disciplines.
- If it is over the number of visits the oasis information provides, they ask people not to see a patient, wait to eval at a later time. They ask me to drop some visits.
- Due to PDGM and coding, it limits how many visits we can have and “spilt” between all disciplines.
This is not the norm, though, at least according to this survey: 64% of home health SLPs don’t work for agencies that limit their number of visits.
Comments from SLPs without agency limits
64% of home health SLPs report their agency doesn’t limit the number of visits they can do. Here are some comments:
- None.
- They give me autonomy.
- No limits. It is at our discretion.
- My frequency/duration is never questioned.
- No limits….have a company model with recommendations, but I put what the patient needs and never get kickback from management.
- Up to 6 + eval unless I write medically appropriate justification.
- My agency doesn’t limit, they trust my judgment and support treatment.
- My company gives suggestions of therapy visits based on the Oasis scores. However, they always tell me to schedule what is right for the patient and typically back me up.
- My agency is pretty good about this. They get a preset number recommendation from Medalogix but if I can explain and justify my reasoning, they’re good with it.
- None! I’m lucky!
That last comment (“I’m lucky!”) really shines a light on this situation, doesn’t it? I’m not an expert on regulations, but from an ethical standpoint, our agencies should support their clinicians providing medically-necessary, skilled intervention. Could you imagine your doctor saying that they’re “lucky” they can see you when you get sick?
Enough to meet patients’ needs?
The number of visits doesn’t directly correlate to meaningful outcomes. We don’t necessarily need a ton of sessions to provide good outcomes, at least for some patients. I’ve written about a couple of them, like this one and this one. But every patient is different, and I’ve worked with a few of my patients for 6 – 8 months to obtain reasonable outcomes, such as this one.
So I asked the home health SLPs to report if the number of sessions they could offer was sufficient to meet their patients needs:
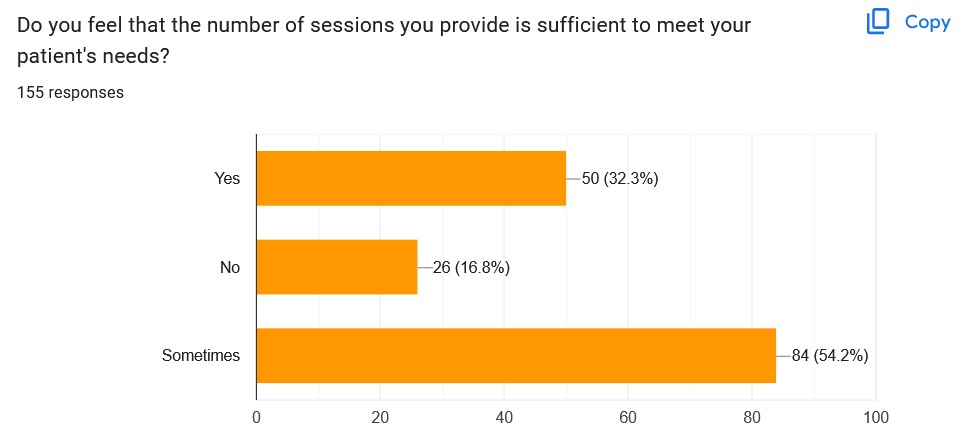
Here, we can see that 32% said “yes,” 17% said “no”, and 54% said “sometimes.”
As you can imagine, there are a number of reasons why patients don’t show meaningful improvement, including patient factors, insurance and agency limits on number of visits, and lack of time during the session to address ST goals.
It’s obvious that home health SLPs face a number of challenges that we don’t have direct control over, but maybe there is a way we can improve the situation by changing how we practice.
Improving participation-focused intervention
My goal this year is to improve my clinical practice by learning and implementing participation-focused interventions. Until a few months ago, I *thought* I was providing participation-focused intervention, but I wasn’t!
While there are some constraints that may forever be out of our ability to influence, I think we do have the ability to improve patient outcomes by providing very targeted intervention. This could allow us to be more effective with fewer visits, if that’s the situation we’re in.
But even if we have “unlimited” visits, we can still improve patient satisfaction and outcomes by focusing on their participation goals. Improving our practice should improve our own satisfaction and perhaps decrease some of our stress, as well!
Learn more about the surveys
If you’d like to learn more about the surveys, I presented on them in my April 2024 course “What Really Happens When Patients Go Home.” It’s available for CEUs as a recording from MSCC (I’m not an affiliate).
Related Eat, Speak, & Think posts
- 50 questions to ask in a home health SLP interview.
- 17 tips for the new home health SLP.
- Best gear for home health therapists and nurses.
Featured image by Tunagaga on Canva.com.
Lisa earned her M.A. in Speech-Language Pathology from the University of Maryland, College Park and her M.A. in Linguistics from the University of California, San Diego.
She participated in research studies with the National Institute on Deafness and other Communication Disorders (NIDCD) and the University of Maryland in the areas of aphasia, Parkinson’s Disease, epilepsy, and fluency disorders.
Lisa has been working as a medical speech-language pathologist since 2008. She has a strong passion for evidence-based assessment and therapy, having earned five ASHA Awards for Professional Participation in Continuing Education.
She launched EatSpeakThink.com in June 2018 to help other clinicians be more successful working in home health, as well as to provide strategies and resources to people living with problems eating, speaking, or thinking.


Be First to Comment