If you are thinking that home health is a walk in the park after I shared my best day, please read on to learn about my worst day as a home health SLP, from a workload perspective. Here’s an overview of this post:
- Things that can make my day difficult.
- A word about privacy.
- How a long day quickly turned into my worst day.
- My worst day as a home health SLP.
- Not my typical day.
Things that can make my day difficult
- The patient is in distress when I arrive.
- The patient has had a fall, with or without injury.
- There is a change in medication.
- The patient is not home or refuses treatment.
- Little actual therapy accomplished during the session.
- New evaluation is in unsafe or unsanitary home.
- More than one non-routine visit, which means significantly more paperwork.
- Having to make multiple phone calls on behalf of patient.
- Driving long distances between patients (my longest is a little over an hour).
All of the above comes with the job, and I embrace it because this is real life. My patients are often pretty sick, and life is messy. I think from Medicare’s perspective (based on how they rate home health agencies), my primary role is to keep patients out of the hospital and to improve their ability to safely function at home.
But I have to admit that when session after session is tough or brings a lot of extra work at the end of the day, it is mentally and physically draining. Usually I don’t have more than one or two tough sessions in a day. Sometimes, there are stretches of a week or more where every day is challenging. That’s when I ask myself if it would really be so bad to quit and go work in a quiet bookstore. (And that’s when I start planning my next vacation.)
Just to be clear, I’m writing about a tough day from the position of workload. I have had emotionally-tough days as well, related to patients in distress or other challenging situations.
A word about privacy
The day I describe below is a day that actually happened, in spirit. I don’t keep records for very long, due to privacy concerns, so I can’t be sure I’m describing the exact 4 visits from that day. However, I distinctly remember scheduling myself a moderately challenging day with the 4 types of visits described below. Next thing I know, my schedule morphed into a really tough day.
The visits I describe below are real situations with real patients. I’ve changed a few details to protect privacy, in case they or anyone they know were to read this.
How a long day quickly turned into my worst day
When I woke up that day, I knew it would be longer than usual. In addition to two routine visits, I had a re-certification and a 30-day re-evaluation scheduled.
7:30 am – Home office
I started up my work laptop and checked email and messages on my work phone earlier than I usually did because I planned to stop by the office before heading to my first patient.
Unfortunately, I discovered one of my patients (a routine visit) was sent to the hospital. I wasn’t given any specific details, but I hoped nothing was seriously wrong and that she would be home soon. In the meantime, I had to fill her spot to meet my productivity requirement.
The second problem I discovered is that the son of one of my other patients texted me to cancel this day’s session (the other routine visit). I called the son to see if they wanted to reschedule for later in the week. They didn’t. This meant I had to notify the doctor that the session was missed for the week, cancel the session in the EMR, and document the situation in a case communication note.
Now I had 2 visits to fill. I checked my schedule for the rest of the week to see if I could move any routine visits to this day. Unfortunately, for one reason or another, I couldn’t move anyone up.
That meant I’d have to take 2 new evaluations, on top of my re-certification and a 30-day re-evaluation. This was going to be a very long day.
My worst day as a home health SLP
8:00 am – Still in the home office
With one nervous eye on the clock, I spent a good 25 minutes scheduling the new evaluations and moving my other 2 visits around to accommodate everyone. I only had time to prepare for my new evaluations by looking at the main diagnosis to get a hint as to what I might find and to make sure I didn’t need insurance pre-authorization.
As a rule, I read through the case history so that I understand what is going on before I meet new patients. I felt bad that I didn’t know the situation before going out, but I had no choice. Time was passing, and I had to finish getting myself ready for work.
9:00 am – Car
No time to stop by the office to check my inbox, turn in paperwork, restock, or make copies. I also wouldn’t be paid mileage to my first patient who lived 30 minutes away. I left home for my first patient. On the way, I listened to the first half of a continuing education course from SpeechPathology.com.
9:30 am – First visit (30-day re-evaluation)
My first visit was to see a middle-aged woman who had had a stroke following surgery for brain cancer. She was severely apraxic and aphasic, meaning that she had severe problem speaking and understanding speech. We had been doing a Lingraphica trial for an augmentative and alternative communication (AAC) device. In addition, we were focusing on verbal scripts, including using video-assisted speech therapy (VAST) on her smart phone.
I started the re-assessment in our previous session, using the Western Aphasia Battery – Revised (WAB-R). We finished the test this day. I was encouraged that her verbal skills had improved over the past month, but functionally, she was still quite limited. I emphasized the gains she had made, including successes her family had shared.
I felt sure that she was aware of how poorly she did on some of the tasks, so I purposely followed up with a task she excelled at. Even though we ended the session on a laugh, I wondered if I could be doing something differently that would be better for her.
I wasn’t able to document anything more than vital signs and pain, and I knew it would take a good hour to write up this visit.
10:30 am – Car
I left her house to drive 30 minutes to my next patient, stopping on the way for a bathroom break and a quick snack. Then I called the doctor to report that one of my patients had cancelled a visit for today. I wanted something a little easier to listen to than finishing my CEU course, so I practiced an audio Chinese lesson through Pimsleur (an on-again, off-again hobby) as I drove to my next patient’s house.
11:10 am – Second visit (new evaluation)
I knocked on the door of one of my new evaluations, knowing only the name, age, insurance, and diagnosis of amyotrophic lateral sclerosis (ALS or Lou Gehrig’s disease). I met my new patient and her son, conducted the interview, and made my plan for evaluation.
My new patient was in her 80’s and had been diagnosed with ALS a year ago. She was bed-bound and totally dependent for care. She was only drinking small amounts for pleasure and received her nutrition and hydration via a feeding tube. Unfortunately, her vision and hearing were severely impaired, and she was unable to talk.
She had started an assessment for an AAC device controlled through eye-gaze several months ago at an ALS clinic. Unfortunately, she had been unable to return to the clinic due to extreme difficulty leaving home.
Her son, understandably, wanted a better way for his mother to communicate. His mother could indicate “yes” and “no” with head movement and had good facial expressions, like smiling and frowning. But she could not ask questions or make requests or comments. It was very frustrating to try to communicate about most things.
The interview alone took half an hour. Then I assessed vital signs. I confirmed that “yes” and “no” were consistent, but only for basic questions that were personally-relevant to the patient.
I decided to set up a joint session with the vendor from Tobii Dynavox and continue the assessment with an eye-gaze controlled AAC device. After discussing the plan with my patient’s son (and directing my comments towards my patient as well), I called the vendor and left a message. Then I called the doctor to report the evaluation and plan of care, and had the son sign the paperwork to continue speech therapy (ST) intervention.
I was not able to write any part of the report, other than vital signs and notes. I knew that this visit would take at least an hour to write up.
12:40 pm – car
I walked out of my second patient’s home asking if it were 5 o’clock yet. Before driving to my next patient, I took a 10 minute break. I found a Dunkin Donuts on the way to the highway for a bathroom break, checked my work email, and just closed my eyes for a few minutes.
Then I drove 30 minutes to my next patient, while listening to a fun episode of “Reply All” – a podcast that solves mysteries about how the internet works.
Check out my post listing 24 podcasts for medical SLPs.
1:30 pm – Third visit (re-certification)
I arrived to see my third patient for the day. I’d only been working with this woman for 3 weeks. ST was ordered late in the case, for memory and executive function difficulties that slowly became apparent to the other disciplines over the course of their treatment. We’d made decent progress, but I wanted to continue for another month. Since all the other disciplines had discharged her, I had to complete the re-certification.
Nursing had recently discharged the patient, so I expected our medication list to be up-to-date. However, I found a few discrepancies between what my patient had in her house and what was listed in the electronic medical record (EMR). Since she had dozens of medications (including creams, ointments, and over-the-counter bottles), I spent a good 25 minutes finding the problems. Then I called our nurse supervisor to take all the information so that he could update our EMR and/or call her doctor to reconcile the problems.
I also completed all the other re-certification tasks described in my previous post, including calling the doctor for new orders to continue ST.
Luckily, I had completed most of my re-evaluation tasks during the previous session. It didn’t take long to finish the re-assessment and discuss goals for the next 4 weeks.
That visit lasted an hour and a half, and again, I was only able to complete a small percentage of the documentation during the visit. I knew it would likely take an hour and a half to write up this visit.
3:00 pm – Car
I left this patient’s house, wistfully thinking of those days when I was done seeing patients around 3:00 pm. Since I was passing by my own house on the way to my final visit, I stopped in to use the bathroom, ate a few small “energy bites”, and brushed my teeth.
Feeling a bit refreshed, I drove on to see my last patient about 10 minutes away. I left the radio off in order to reflect on the day so far and mentally prepare for the final visit.
3:30 pm – Fourth visit (new evaluation)
I arrived for my second new evaluation that day, with little idea why ST was ordered for this older gentleman with Parkinson’s disease. I treat a lot of people with this condition, so I had a good idea what to expect.
Once I’m sitting down with him, I peeked at what the nurse had written. She reported that he had complained about coughing on water. As I interviewed him, it became apparent that his speaking ability was impaired (dysarthria) and he had concerns about a decline in memory as well. I wasn’t surprised since it isn’t rare for people with Parkinson’s to have difficulties in all three areas (swallowing, communication, and cognition).
Since I didn’t have time to assess everything during that session (and it would have been too much to ask of him), I assessed swallowing. First, I administered the EAT-10 and the Reflux Symptom Index (RSI). Second, I completed the oral mechanism exam to see how the parts of his mouth were working. Finally, I conducted a clinical swallow evaluation.
I recommended a modified barium swallow study (MBS study) from the mobile company we often refer to. After discussion, we decided to assess voice at the next session to see if he would be a good candidate for LSVT LOUD. We would assess cognitive communication skills at the following session. If he was a candidate for LSVT LOUD, we would hold off on formal cognitive intervention until next month. I would be sure to incorporate cognitive exercises into the LSVT LOUD program, as long as it didn’t impede his progress.
I called his doctor to request a verbal order for ST and had my patient sign the paperwork to update his plan of care.
As with every session this day, I was barely able to document more than vitals and pain and take notes. I knew that this session and the MBS study referral form would take a solid hour, if not longer, to write up.
4:45 pm – Car
I climbed back into my car for the 10 minute drive home. I drove home in silence as the day reverberated through my head.
4:55 pm – Home
I arrived home tired and hungry, so I steamed some vegetables and supplemented with leftovers and sat down to relax for half an hour. Then I took a 10 minute walk around the block to clear my mind a little.
5:35 pm – Home office
I turned my laptop back on and spent a solid 35 minutes reading and responding to work emails.
6:10 pm – Finally start documenting
I knew I had at least 4.5 hours of documentation ahead of me. We are supposed to complete documentation within 24 hours. I knew I wouldn’t finish completely, but I wanted to get as much done as I could. I started with the re-certification since it was essential for billing that this visit be written up as soon as possible.
9:30 pm – Stopped for the night
I wasn’t completely done, but frankly I was exhausted. I’d been working since 7:30 am. I was also thankful that this day wasn’t worse. My patients were relatively close together, no one was in distress, and no one had fallen. Neither of my new patient’s homes appeared unsafe or unsanitary. We were able to make solid progress during each session.
I went to bed reassured that the next day didn’t look very challenging. But we all know now how fast things can change in home health!
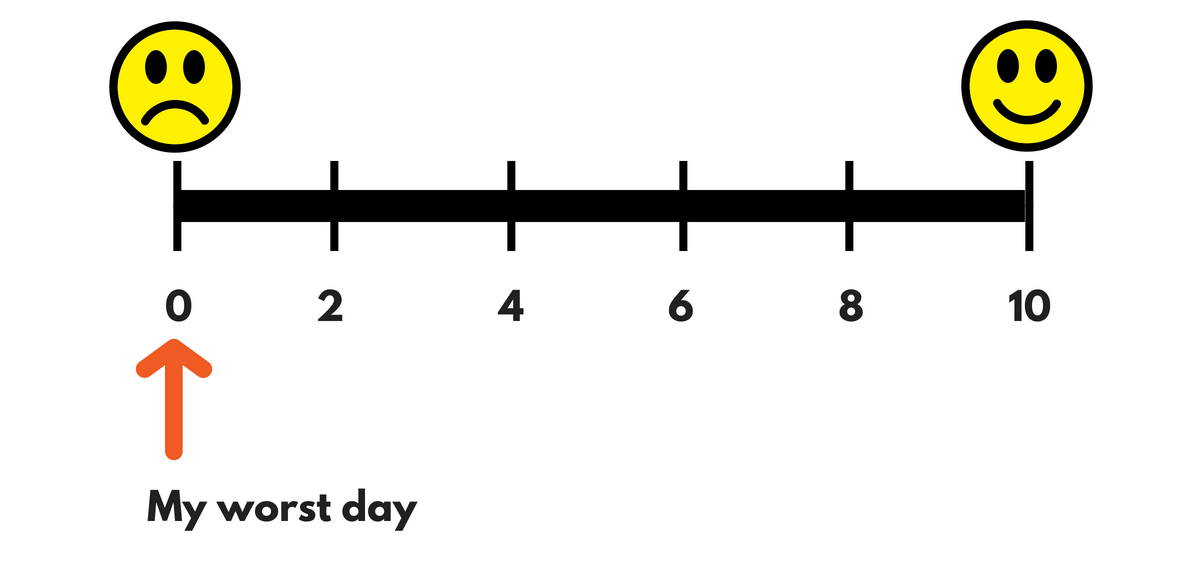
Not my typical day
I know every home health SLP has a different overall experience due to a variety of factors. I can only speak from my own experience, but thankfully this is not what my normal day looks like. Sadly, my normal also doesn’t look like my best day as a home health SLP. As you can imagine, most of my days are somewhere in between.
Read the 5 big-picture strategies I learned which improved my work-life balance, and how organizing your work bag can save you time.
If you are a home health therapist, what was your worst day like? Leave a comment below.
Lisa earned her M.A. in Speech-Language Pathology from the University of Maryland, College Park and her M.A. in Linguistics from the University of California, San Diego.
She participated in research studies with the National Institute on Deafness and other Communication Disorders (NIDCD) and the University of Maryland in the areas of aphasia, Parkinson’s Disease, epilepsy, and fluency disorders.
Lisa has been working as a medical speech-language pathologist since 2008. She has a strong passion for evidence-based assessment and therapy, having earned five ASHA Awards for Professional Participation in Continuing Education.
She launched EatSpeakThink.com in June 2018 to help other clinicians be more successful working in home health, as well as to provide strategies and resources to people living with problems eating, speaking, or thinking.


There are some interesting points in time in this article. There is some validity but I will take hold opinion until I look into it further. Good article, thanks and I want more! Added to my Feed as well.
[…] My worst day as a home health SLP. […]