If you’re curious about what it’s like to be a home health speech-language pathologist (SLP), I’m going to share my best day as a home health SLP. (I’ve also written about my worst day, from a workload perspective). Of course, most days are a mix of good and difficult. Here’s what I’ll cover:
- Things that make my day go well.
- A few things to know about my job.
- My best day as a home health SLP.
- Stay tuned for my worst day as a home health SLP.
- Read what other home health therapists have written.
Things that make my day go well
- Meaningful success with a patient.
- Productive sessions.
- Connecting with a patient and family.
- Sharing a laugh or bringing comfort.
- Receiving compliments or thanks.
- Short travel times between patients.
- Finishing documentation during or between session.
- Making a presentation in the community or giving an inservice.
- Benefiting from support from management.
A few things to know about my job
- I’m paid for 24 hours a week.
- Productivity is 16 visits, which I spread over 4 days.
- Productivity is only adjusted for meetings and authorized activities.
- I drive my own car and earn mileage.
- I cover 19 cities and towns in central Connecticut.
- I set my own schedule, and generally can see patients anytime during a full week.
- I don’t open cases (SOC’s), but I do plenty of recertifications, transfers, and discharges.
- My company only provides the WAB-R and the old CLQT. I buy all the other assessment and therapy tools I use.
- My company encourages setting frequency and duration according to clinical need.
My best day as a home health SLP
“Best day” can mean either great outcomes for a patient or a smooth, easy day. I’m going to talk about the easiest day I’ve had in the past nearly 4 years in home health, since my focus is on what it is like to be a home health SLP.
Last week, I had the easiest day ever. It was possible because I currently have several patients in my hometown, which is rare. Here’s how my day went.
8:00 am – Home office
I turned on my work laptop and read through email. Only two required a response. I updated the electronic medical record (EMR) program and checked for updates on my patients. I checked my work phone – no new messages.
I also ran through my patients for the day and made sure I had what I needed for our sessions. Then I spent 15 minutes working on a future blog post before finishing getting ready to leave.
9:05 am – Car
I left for my first patient who lives about 7 minutes away.
9:15 am – First routine visit
My first patient was an elderly woman in an assisted living facility who I know from previous therapy for cognitive-communication deficits. She had a recent hospitalization for an unrelated condition and was referred to speech therapy (ST) at her request for memory and word finding problems.
The nursing staff didn’t notice a decline, but her son noticed a decline in memory for recent conversations and word finding. I had noticed during the evaluation last week that she was more disorganized than she was when I last worked with her the previous summer.
This day, we focused on organization and access of important information by working together to update her memory binder and rehearsing how to find information. During the session, I was able to fill out most of my visit note. We ended the session at 10:00 am and I sat in the lobby to finish her note before I used the restroom and left.
10:20 am – Car
For the next 15 minutes, I ate a mid-morning snack and checked work email, personal email, and social media. Then I started my 15-20 minute drive to my next patient.
11:00 am – Second routine visit
My second patient was a woman in her early 90s who lives at home with a 24-hour paid caregiver. Her daughter was present for nearly every session. I picked her up for swallowing and memory.
For swallowing, she had been coughing with food. I had her do a modified barium swallow study (MBS study) a few weeks earlier through MassTex Imaging, a mobile service, which I was able to attend. Luckily, she only needed to have a chin-down position for mastication and swallowing. Three weeks later, she continued to use the strategy and was no longer coughing with food.
We were still working on memory, and I was planning to discharge soon. My overall goal was to find a set of exercises or activities for cognitive-linguistic stimulation. My patient was enthusiastic about participating, as were her daughter and paid caregiver. They reported that my patient had become more animated and engaged since beginning speech therapy (ST). Previously, she spent much of her day watching TV or napping. Now, both the daughter and paid caregiver are working with her daily.
My patient also had a specific goal to be able to remember her paid caregiver’s name. It really bothered her that she kept forgetting. So I used spaced retrieval with errorless learning to help her to remember. During delays of 3 minutes or less, we sat in silence which helped with retention. During this time, I worked on documentation. Once the delays were longer, I educated the patient and her caregivers about cognitive stimulation activities and provided written ideas including this great list of cognitively-stimulating activities (moderate complexity) from the Nice Speech Lady.
12:00 pm – Car
I had plenty of time before my next appointment, so I stopped at a dollar store to pick up whiteboards, calendars, binders, and other supplies for executive function therapy. My company does not reimburse me, but I know that many of my patients either cannot physically go to the store, won’t buy the right thing, or can’t afford to buy extra things.
As I drove to my next patient, I drank an Ensure and ate a clementine and a few vegetable sticks. Last month, I switched from IsaGenix shakes to Ensure after talking to a dietician and an athletic trainer. I don’t like to eat heavy food mid-day now that I’m sitting most of the day.
12:30 pm – Independent living building
I had 30 minutes before my next session, so I sat in a quiet lounge across the hall from my next patient. I completed my documentation from my second session this morning, and then caught up on work email. I had time to check my personal phone, stretch, and use the restroom before seeing my next patient.
1:00 pm – Third routine visit
My next patient was an older woman who had had a significant recent decline in cognition. I just picked her up last week. We had several functional goals to work on, but the primary goal for this week was to focus on remembering to use the walker.
She forgets to use her walker inside the apartment, even though she has significant pain in her hip when she doesn’t use it. She readily says that she knows she should use the walker, and that her hip doesn’t hurt when she uses it. But I’ve seen her get up and walk across the living room without the walker, wincing with every step.
This day, I used spaced retrieval with errorless learning to help her to automatically reach for the walker when she stood up. She made nice progress, and she was very appreciative. Because there was a lot of down time due to using spaced retrieval, I finished my note by the time I left.
2:00 pm – Car
I stopped in the restroom on my way out of the building. My next patient was in another building on the same property, so I had plenty of time before our 2:30 pm appointment. It was too hot to take a walk, so I sat in my car and ate a filling snack. I called my grandmother and chatted with her for 10 minutes. I quickly checked my work phone and personal phone, then I headed over to my last patient.
2:30 pm – Fourth routine visit
My last patient was another lovely woman in her 90s. She recently reported difficulty swallowing and she had been missing medical appointments. I evaluated her last week for swallowing and cognitive-communication skills.
For swallowing, she complained about food getting stuck in her throat. I assessed her with her normal lunch which included regular, mixed, and soft consistencies. I noticed what seemed to be mildly prolonged mastication but no other significant signs of dysphagia. I suspected a pharyngeal and/or esophageal issue, so I recommended an MBS study from the mobile company. I told her at this day’s session that the MBS study would take place tomorrow, and she was happy to hear that.
For cognitive-communication, she had been missing doctors appointments, reduced orientation to time, increased difficulty using the calendar, and increased disorganization. She was not fully accepting that she was having these difficulties. Today, I asked open-ended questions and paid attention to the specific words she used when expressing her challenges. Then I only used those words to describe the assessment and treatment process. She agreed to start a cognitive-communication assessment this day.
I began the Ross Information Processing Assessment – Geriatric Version 2nd Edition with her. We finished the first 5 subtests. Because she wanted to know how she did, I scored those subtests while sitting with her. I also knew that this would make writing up her visit that much faster.
3:30 pm – Car
My last session was over, and I had a short seven-minute commute home.
3:40 pm – Home
I plugged in my laptop and finished writing my last visit note. I checked work email again, updated the EMR for my travel time and non-session time, and emailed my productivity to my supervisor.
4:00 pm – Officially done for the day
I’m rarely done with work by 4 pm – it’s a great feeling!
Stay tuned for my worst day as a home health SLP
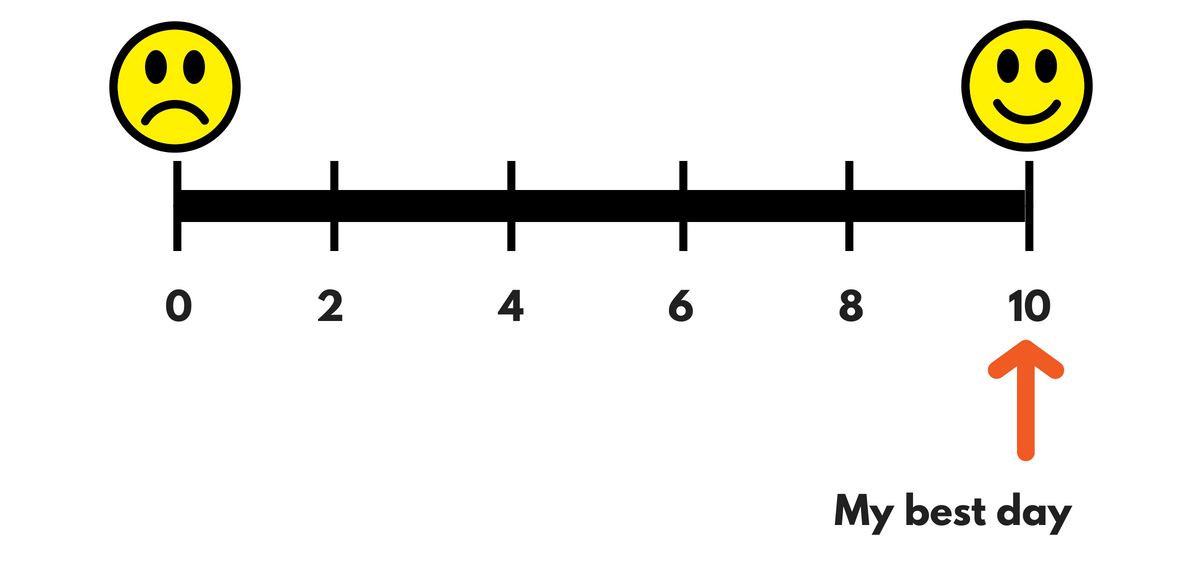
If only all of my days went so smoothly! Next week, I’ll share my worst day as a home health SLP. As you can imaging, most days are somewhere in the middle between those two endpoints on the spectrum. [Update: While writing about my worst day, I realized I needed to first explain about how we assess holistically at each session and the 8 different types of visits we have to document.]
If you haven’t already, sign up for my newsletter so you won’t miss out. I’ll send the email newsletter once every other week, and it will include:
- links to new posts on Eat, Speak, & Think.
- any new free PDF resources.
- links to a few related, interesting things around the web.
- links to a few tools or resources that may interest you as a creator.
You can sign up via the sidebar form or the pop-up form. Contact me if you have any problems.
Read what other home health therapists have written
I’ve read a few other accounts by home health therapists that I’d recommend, in case you’re interested:
- Jenna Gregor, MS, CCC-SLP wrote a blog post on Tactus Therapy about a day in her life as a home health SLP.
- Dysphagia Ramblings wrote “A week as a home health SLP” in a series of blog posts.
- Three home health physical therapists wrote about their experiences in “Is home health rehabilitation for you? Why or why not?“, which ring true with me.
I learn so much from other SLPs. If you’re a home health therapist, please share what your experience is like in the comments below.
Lisa earned her M.A. in Speech-Language Pathology from the University of Maryland, College Park and her M.A. in Linguistics from the University of California, San Diego.
She participated in research studies with the National Institute on Deafness and other Communication Disorders (NIDCD) and the University of Maryland in the areas of aphasia, Parkinson’s Disease, epilepsy, and fluency disorders.
Lisa has been working as a medical speech-language pathologist since 2008. She has a strong passion for evidence-based assessment and therapy, having earned five ASHA Awards for Professional Participation in Continuing Education.
She launched EatSpeakThink.com in June 2018 to help other clinicians be more successful working in home health, as well as to provide strategies and resources to people living with problems eating, speaking, or thinking.


[…] My best day as a home health SLP. […]
Nice Post,
Thanks for the information.